If you are having a vaginal delivery, a non-complicated birth is what you would likely want. But sometimes you and your medical provider may require assistance through forceps delivery. Going into labor is exciting, but it can also be nerve-racking. You are excited to meet your little bundle of joy, but you may also have a million questions running through your mind, like what are forceps, and what is a forceps delivery? These questions are entirely normal, and though you might be informed on a gazillion pregnancy and delivery-related topics, it’s normal to worry about your child’s birth.
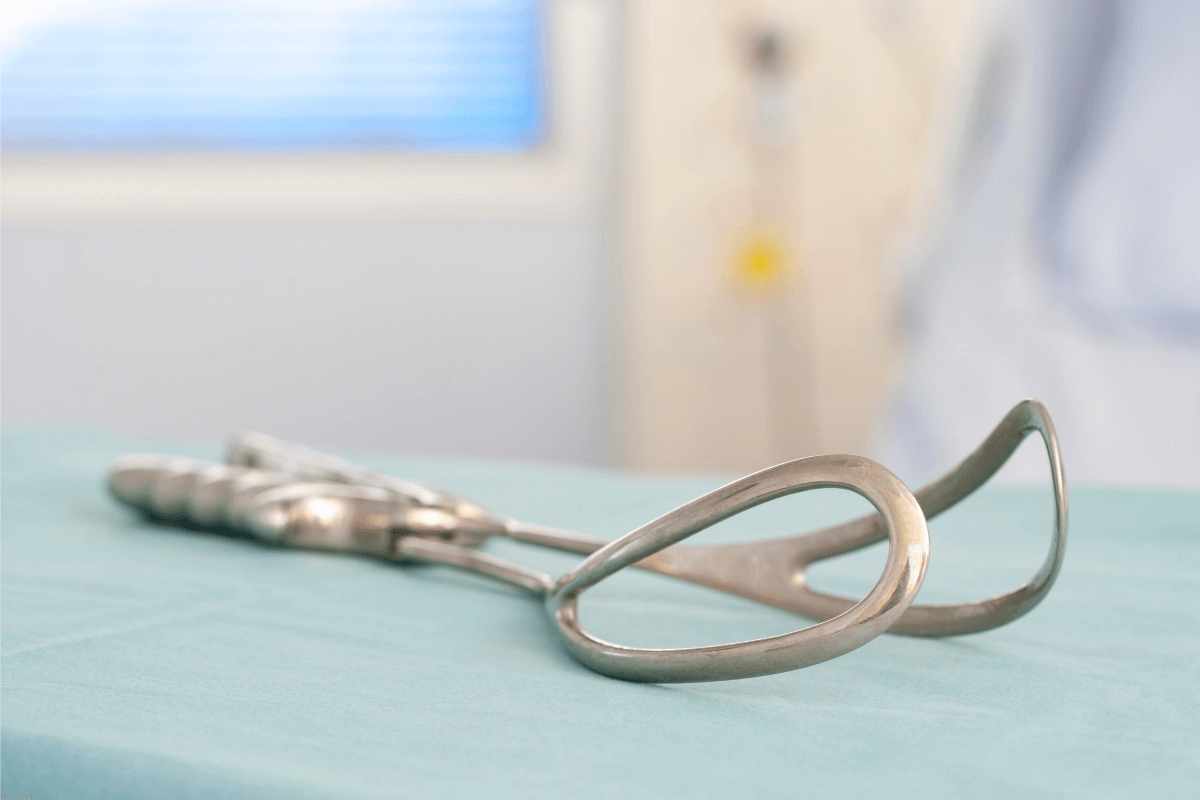
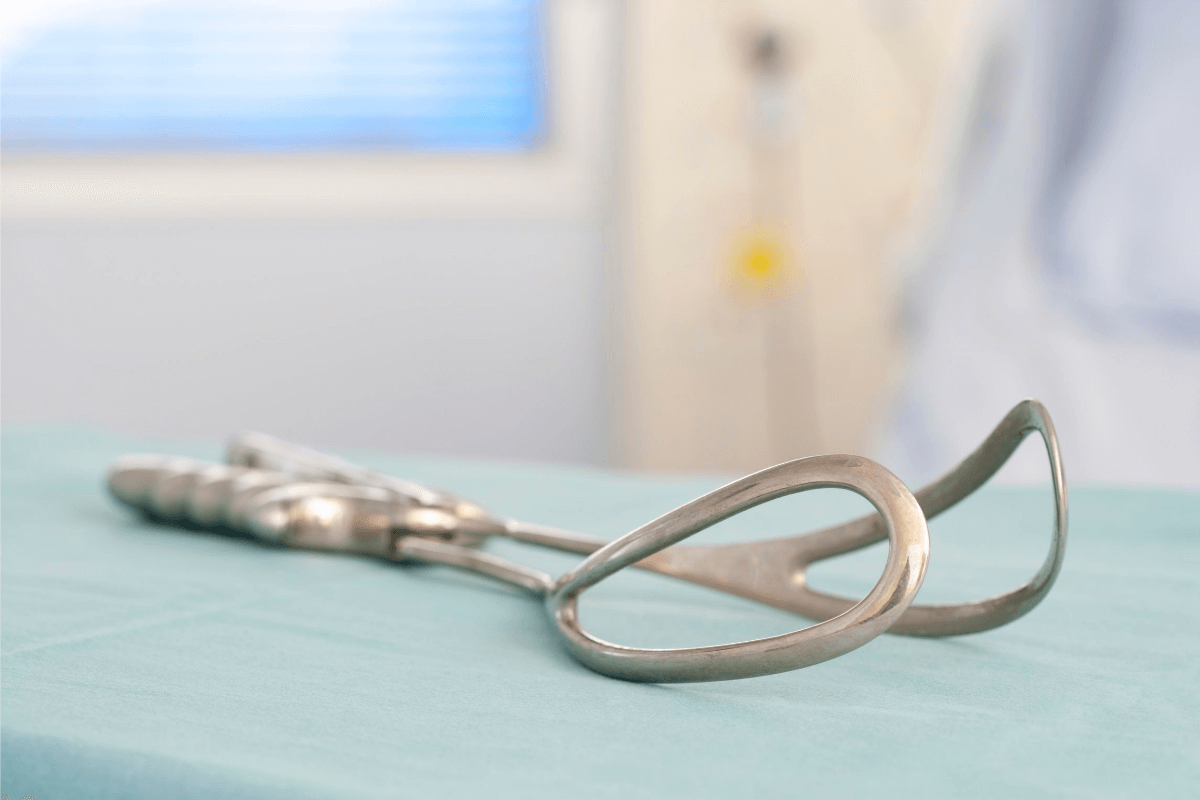
Forceps delivery is a form of operative vaginal delivery involving forceps to deliver the baby. Though there are over 700 different types of forceps, they are classified into three main groups:1,2
- Outlet forceps
- Scalp is visible
- Fetal skull reached the pelvic floor, and the head is on the perineum
- Rotation does not exceed 45 degrees
- Low forceps
- Leading point of fetal skull at >= +2, not on pelvic floor
- Rotation 45 degrees or less (LOA/ROA to OA or LOP/ROP to OP); or rotation greater than 45 degrees
- Mid forceps
- Baby’s head is above +2 centimeters
Typical components of forceps include handles, a lock, shanks, and blades. Though all forceps look similar and have similar features, medical providers use different ones depending on the baby’s position.2
The use of forceps has declined in recent decades, and a study, which took into account 22 million vaginal deliveries from 2005 to 2013, found that forceps were used only in 1.1% of cases. The decline in forceps deliveries has been associated with fears of an increase in the risk of tearing, injury to the baby, and lack of experience among doctors.3
Your medical provider may suggest forceps delivery for several reasons:1,4
- You’re too tired to push anymore.
- Your health history may mean pushing for too long may be a problem.
- Your baby’s heart rate is a concern.
- Your baby doesn’t want to come out, and labor stalls.
A forceps delivery isn’t a choice your doctor can take lightly due to the increased risks of injuries. Hence specific criteria must be fulfilled to go ahead with it. The following criteria are recommended for a forceps or vacuum-assisted delivery to take place:3
- Complete dilation of the cervix.
- Membrane rupture
- The head of the fetus is engaged.
- The fetal position is known.
- There’s an estimate of the weight of the fetus.
- Mom’s pelvis should be adequate for the baby to pass through.
- Administration of anesthesia.
- The mother’s bladder is empty.
- Consent is given with an explanation of the risks and benefits.
- A backup plan is in place.
- When pushing isn’t feasible, the mother has a cardiac or neurologic disease.
Depending on the baby’s position, your provider will select the proper pair of forceps for the procedure. The fetus naturally undergoes a set of movements to negotiate the birth canal called cardinal movements. There is some professional disagreement on whether there are seven or four of these cardinal movements, which include engagement, descent, flexion, internal rotation, extension, external rotation, and expulsion.1,5
If the fetus does not complete all the cardinal movements, your provider can use forceps to help it. For example, if your baby only engages your pelvis, it will need help completing the rest of the movements to descend through the birth canal.
If all the conditions for a forceps delivery are complete, your provider can begin helping the baby through the birth canal. You’ll continue pushing, and someone will use rest periods between contractions to place the forceps on either side of your baby’s head or feet. They’ll use a contraction to apply gentle traction with the forceps to guide the baby out while you push. Your provider may also perform manual rotation to get the baby in an appropriate position.1
Forceps delivery isn’t risk-free, though it does have many benefits, which has led to doctors calling for training in obstetrics to use forceps.
Evidence suggests the use of forceps in deliveries is associated with a lower failure rate than a vacuum. Using forceps also means a Cesarean section isn’t performed, which means less time in the hospital compared to a woman who has undergone a C-section and a faster recovery time. Another significant benefit is that forceps can come in handy when a baby needs to be delivered quickly, as in the case of fetal distress.2
Trauma due to the use of forceps can occur to the mother or the fetus. Maternal trauma includes increased perineal and vaginal trauma such as third or fourth-degree tears, urine and fecal incontinence, hematomas, and long-term complications of pelvic organ prolapse.3
Fetal trauma includes injury to facial nerves, trauma to the skull and brain (skull fracture and intracranial hemorrhage), and even death.3
Despite forceps and vacuum delivery being operative vaginal deliveries, they have considerable differences and benefits.
The advantages of forceps over vacuums include the following:2,3
- Faster delivery of a fetus in distress
- Lower failure rate
- Unlikely to detach from the fetus’s head
- Allows rotation of the fetus
- Less encephalopathy and bleeding from the scalp
- Fewer cases of cephalohematoma
- Fewer cases of retinal hemorrhage
- It can be used in premature fetuses
The disadvantages of forceps include:2
- Stronger anesthesia is needed for the mother.
- Facial bruising and injury to the facial nerves resulting in paralysis palsy are more common while using forceps.
- Greater perineal trauma, which means trauma to the mother’s genitalia.
Delivery assisted by a vacuum is generally better for the mother, whereas delivery assisted by forceps is usually better for the fetus.3
Recovery from a forceps delivery is usually shorter than a C-section and about the same time as an unassisted birth which is why there are calls to train medical professionals to use forceps. Forceps can also prevent other complications due to a C-section, such as infection, repeat Cesarean sections and pain.
Forceps delivery can cause tearing, so appropriate measures must be taken to prepare to suture the lacerations while preparing for the delivery itself. Severe tearing may take longer to heal.1
The use of forceps delivery has declined over the years, and not all hospitals or medical colleges train physicians and students to use forceps, leading to its decline. It is essential to ask your medical provider if they are trained in using forceps for delivery in case you need to undergo this procedure. A trained professional can ensure the best possible outcome for you and your baby.

 PARENTING TIPS
PARENTING TIPS PREGNANCY
PREGNANCY BABY CARE
BABY CARE TODDLERS
TODDLERS TEENS
TEENS HEALTH CARE
HEALTH CARE ACTIVITIES & CRAFTS
ACTIVITIES & CRAFTS