A University of Texas at Arlington bioengineer and his doctoral student have discovered how to identify which brain cells lead to epileptic episodes in children.
Professor of Research Christos Papadelis and doctoral student Ludovica Corona, who is first author, have written a paper published in Brain, a highly touted scientific journal. The study, “Non-invasive mapping of epileptogenic networks predicts surgical outcome,” is supported by UT Arlington and Cook Children’s Health Care System and funded by the National Institute of Neurological Disorders and Stroke and was produced in collaboration with Boston Children’s Hospital, Massachusetts General Hospital and Harvard Medical School.
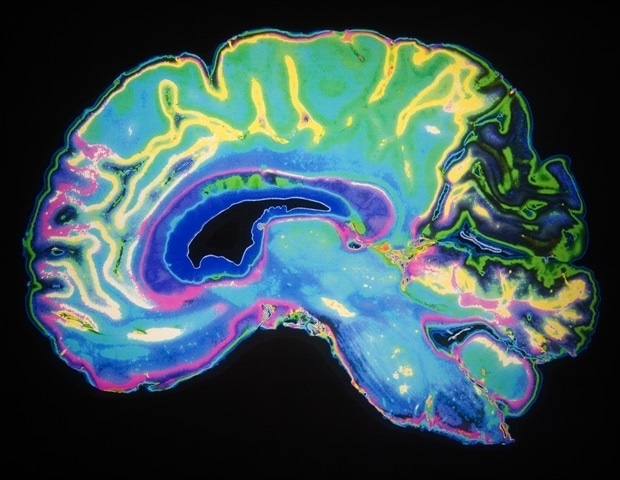
Papadelis and his team used noninvasive techniques and advanced computational methods to measure the electric and magnetic signals generated by neural cells in the human brain and identify functional networks that are responsible for the generation of seizures in children suffering from epilepsy. This new method identifies those functional networks with high precision.
“This could benefit so many children who can’t control epilepsy with drugs, which represents between 20 and 30% of children suffering from epilepsy,” said Papadelis, who also serves as the director of research in the Jane and John Justin Neurosciences Center at Cook Children’s Health Care System.
Currently, Papadelis said, epilepsy surgery is the safest and most effective treatment for these patients since it offers a 50% chance of eliminating seizures.
“By identifying which parts of the brain are producing the seizures, we can then resect them with brain surgery or ablate them with laser,” Papadelis said. “The test we developed pinpoints exactly where the epilepsy network is occurring. Currently, there is no clinical exam to identify this brain area with high precision.
“Seizures affect these children throughout their entire live and have significant impact in their normal development. Successful treatment of epilepsy through surgery or laser ablation early in life would provide an improved outcome for these children since their brains possess extensive neural plasticity and can recover after surgery better than adult brains. This would help the children live seizure-free and have less comorbidities from epilepsy.”
Epilepsy is a common neurological disorder affecting about 3.4 million people in the United States. Of those, about 470,000 are children, or about one of every 100 children in the U.S. Children with uncontrolled seizures are at increased risk for poor long-term intellectual and psychological outcomes, along with poor health-related quality of life.
Michael Cho, chair of the UTA Department of Bioengineering, said this research is a characteristic example of how bioengineering research can have a direct impact on the lives of patients.
This research has real promise. In many areas, the quicker and more accurately the problems are detected and solved, the better chance patients have of living normal lives. The diagnostic tool is great in that it is non-invasive as well.”
Michael Cho, Chair of the UTA Department of Bioengineering
Source:
University of Texas at Arlington
Journal reference:
Corona, L., et al. (2023) Non-invasive mapping of epileptogenic networks predicts surgical outcome. Brain. doi.org/10.1093/brain/awac477.

 PARENTING TIPS
PARENTING TIPS PREGNANCY
PREGNANCY BABY CARE
BABY CARE TODDLERS
TODDLERS TEENS
TEENS HEALTH CARE
HEALTH CARE ACTIVITIES & CRAFTS
ACTIVITIES & CRAFTS