In a recent study published in eBioMedicine, researchers evaluated the relationship between attention-deficit/hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) symptomatology and the cord blood lipidome at the age of two years.
They also determined the relationship between prenatal and perinatal ASD and ADHD estimators and the cord blood lipidome.
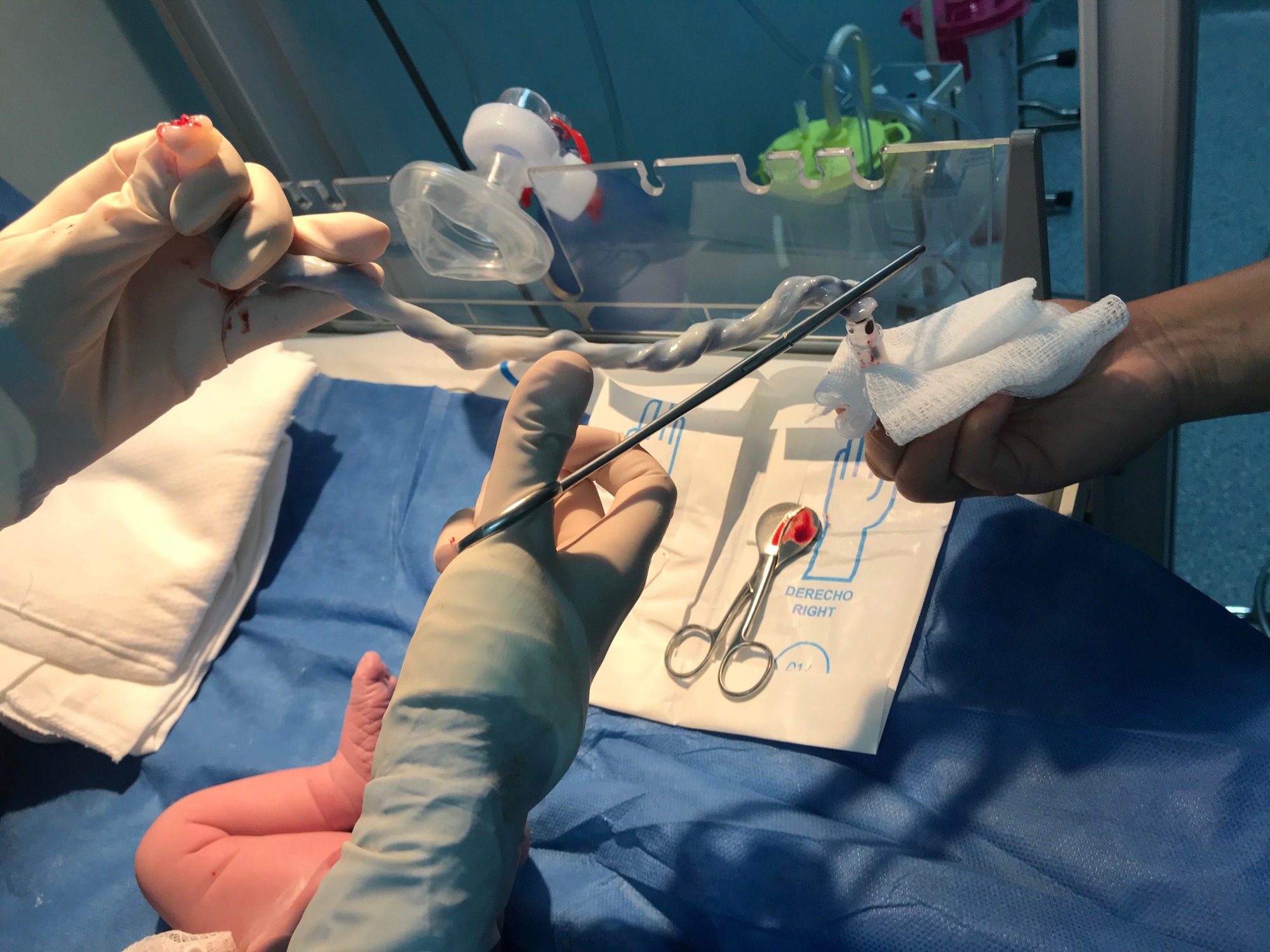 Study: Cord blood lipid correlation network profiles are associated with subsequent attention-deficit/hyperactivity disorder and autism spectrum disorder symptoms at 2 years: a prospective birth cohort study. Image Credit: LOLA61/Shutterstock.com
Study: Cord blood lipid correlation network profiles are associated with subsequent attention-deficit/hyperactivity disorder and autism spectrum disorder symptoms at 2 years: a prospective birth cohort study. Image Credit: LOLA61/Shutterstock.com
Background
Early-life risk factors like contaminant chemicals and maternal inflammation affect neurodevelopmental conditions such as ASD and ADHD.
These conditions can lead to changes in serological lipids, which are crucial for neurodevelopment and constitute 50–60% of brain weight (dry). However, research on lipid metabolism and lipid profiles in early neurodevelopmental disorders is limited.
The Barwon Infant Study (BIS) reported that impaired calorie metabolism at week 28 of gestation is related to ASD symptoms at the ages of two and four years, indicating that lipid profiles are potentially crucial to ASD and ADHD.
About the study
In the present prospective birth cohort study, researchers used lipidomic analysis data from the BIS study to investigate the relationship between cord blood lipids and ASD and ADHD symptomatology at the age of two years.
They also evaluated the association between pre- and peri-natal factors and ASD and ADHD and the extent of mediation of the association by cord blood lipids.
The BIS cohort of 1,074 mother-infant dyads in Victoria, Australia, analyzed infantile lipids in blood at delivery by ultra-high-performance liquid chromatography-tandem mass spectrometry (UHPLC-MS).
The researchers clustered lipids into lipid modules through weighted gene correlation network analysis (WGCNA).
They performed multivariate linear regressions to explore associations between the modules and ASD and ADHD symptoms at two years, adjusting for child age at assessment, sex at birth, time to serum freeze, time in the freezer, and maternal cord blood contamination.
The team performed mediation analysis to evaluate the indirect impacts of prenatal as well as perinatal factors that increase ASD and ADHD symptom risk through the modules.
The study recruited individuals from Barwon using antenatal sampling frames from July 2010 to July 2013. The researchers obtained maternal blood at week 28 of gestation and umbilical cord blood at birth. In addition, they collected infantile venous blood and assessed cord blood for maternal blood contamination by analyzing deoxyribonucleic acid (DNA) methylation profiles.
The researchers obtained lipid measures from the blood of to-be mothers at week 28 of gestation, cord blood, and infantile blood at six months, 12 months, and four years.
They also assessed targeted metabolomic profiles from maternal and umbilical cord blood and analyzed them by nuclear magnetic resonance (NMR).
In preschool children, the team measured ASD- and ADHD-related symptoms using the Child Behavior Checklist (CBCL) at the age of two years and the Strengths and Difficulties Questionnaire P4-10 (SDQ) at the age of four years.
They obtained prenatal factors from maternal questionnaires, clinical examinations, and antenatal records.
They validated perinatal factors with hospital data, including delivery mode, cesarean birth (planned versus emergency), labor duration, the child’s gender and gestational age at delivery, Apgar scores at five minutes, and birth weight.
Results
The acylcarnitine module was related to ASD and ADHD symptoms at the age of two years. Higher birth acylcarnitine levels partly mediated risk factors for neurodevelopmental outcomes, including household income, maternal inflammation, and Apgar scores. Other umbilical cord blood lipids were also related to ASD and ADHD symptoms.
Nine lipid modules showed significant associations with increased ADHD symptom risk at two years, four of which were also significantly related to increased ASD symptom risk at two years.
The Blue-SMD(hub), Turquoise-PE(hub), and Cyan-AC lipid modules showed the lowest p-values and highest magnitude related to ADHD symptom risk.
For a standard deviation increase in the Cyan-AC, Turquoise-PE(hub), and Blue-SMD(hub) modules, the estimated mean differences in ADHD symptoms at two years were 0.5 points, 0.4 points, and 0.3 points, respectively.
Higher Cyan-AC levels in umbilical cord blood partially regulated the relationship between lower household income during pregnancy and a higher frequency of ADHD symptoms at the age of two years.
Maternal NOPMS and the NOPMS and GlycA at birth were associated with ADHD symptoms, but maternal GlycA was not. The cord blood lipid profile mediated the relationship between birth factors such as a low Apgar score, birth GlycA, birth non-oxidative pyruvate metabolism, and ADHD symptoms.
Acylcarnitines mediated the relationships between household incomes, maternal NOPMS, GlycA at birth, and ASD symptomatology.
The study identified several lines of evidence for causation, including consistent findings across the two-year CBCL and the four-year SDQ questionnaire subscales that acylcarnitines were related to ASD and ADHD symptoms.
Conclusion
Overall, the study findings highlighted the relationship between the cord blood lipidome and ASD and ADHD symptom risk at the ages of two and four years. Elevated cord blood birth acylcarnitine levels were related to prenatal and perinatal risk factors for ASD and ADHD symptoms in early life.
The findings highlight the importance of lipids at birth in ASD and ADHD pathogenesis and prevention.
Future research could incorporate measurements of carnitine, short-, medium-, and very long-chain acylcarnitines, mitochondrial function, carnitine shuttle transport, and related metabolites to elucidate ASD and ADHD mechanisms in children.

 PARENTING TIPS
PARENTING TIPS PREGNANCY
PREGNANCY BABY CARE
BABY CARE TODDLERS
TODDLERS TEENS
TEENS HEALTH CARE
HEALTH CARE ACTIVITIES & CRAFTS
ACTIVITIES & CRAFTS

