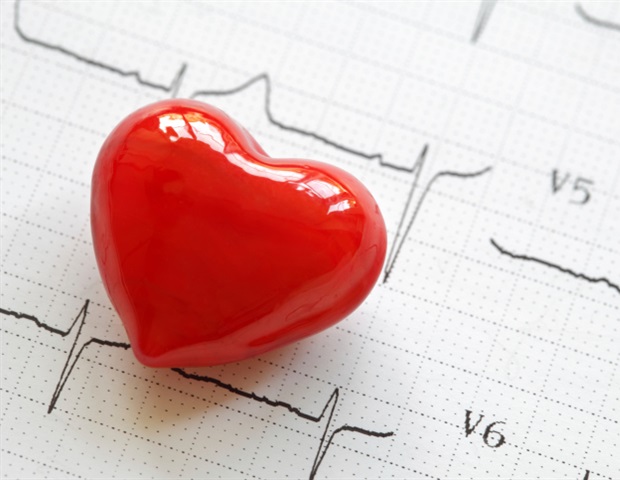
Recent advances in newborn heart surgery have greatly reduced brain injuries in infants with congenital heart disease, according to a 20-year study by scientists at UCSF Benioff Children’s Hospitals and British Columbia Children’s Hospital (BCCH).
The study, begun in 2001 and published this month in the Journal of the American College of Cardiology, analyzed brain imaging data from 270 full-term UCSF and BCCH newborns with congenital heart disease (CHD) for changes in brain injuries before and after newborn cardiac surgery. The scientists confirmed that recent advances in surgical and clinical care that maintain a higher postoperative blood pressure resulted in reduced brain injuries and better chances of patient survival.
We were surprised to find that advances in care over the past 7 years resulted in a clear decline in brain injury linked to increasing the patient’s blood pressure following surgery. With advances in cardiac therapy and outcomes, our focus now is helping these children thrive.”
Shabnam Peyvandi, MD, lead author and pediatric cardiologist for UCSF Benioff Children’s Hospitals
CHD, which refers to one or more abnormalities of an infant’s heart, impacts 40,000 newborns a year in the U.S. It is the most common newborn birth defect. About 1 in 4 of these infants have critical CHD and require surgery in the first month to first year of life. Heart abnormalities include improperly functioning heart valves, a hole in the muscular wall separating the heart chambers, and malformations in the heart’s blood vessels, which can result in altered patterns of blood flow. These anomalies reduce the flow of oxygen and nutrients to the brain and organs before birth and can contribute to lifelong neurological and developmental disorders.
New approaches to monitor brain health
To monitor infant brain health for the study, UCSF and BCCH scientists used advanced magnetic resonance (MRI) brain imaging before and after heart surgery and consistently as the patient aged. The data was divided into four sequential stages, each containing five consecutive years of data. In the fourth and final stage, which ran from 2016 to 2021, infants were maintained at higher post-surgical blood pressures than in previous groups. This resulted in an almost 20% reduction in post-surgical brain injuries compared to the first group in 2001.
During the course of this study, Peyvandi and the UCSF Benioff Children’s Hospitals Pediatric Heart Center published multiple articles investigating brain development and white matter injuries – including a link between moderate-severe white matter injuries that led to delays in childhood motor function – that opened the door to improving long term developmental outcomes by decreasing early brain injuries.
“Taken together, these findings underscore the importance of tracking brain injury and implementing changes to reduce occurrences that will improve outcomes,” said Patrick McQuillen, MD, senior author and professor of Pediatrics, UCSF Benioff Children’s Hospitals. “Based on this research and others, several leading heart centers have incorporated brain imaging into routine clinical practice.”
Work from this group has directly informed the creation of novel clinical programs to monitor and protect the brain in fetuses, newborns and children with CHD, including the Healthy Hearts & Minds Program and the Neonatal Cardiovascular Center of Excellence’s GRowth and NeuroDevelopment (GRAND) program that incorporates developmental care on the inpatient setting for newborns with critical CHD.
Other UCSF authors include Duan Xu, PhD, A. James Barkovich, MD, Dawn Gano, MD, MAS, V. Mohan Reddy, MD
Source:
University of California, San Francisco (UCSF)
Journal reference:
Peyvandi, S., et al. (2023) Declining Incidence of Postoperative Neonatal Brain Injury in Congenital Heart Disease. Journal of the American College of Cardiology. doi.org/10.1016/j.jacc.2022.10.029.

 PARENTING TIPS
PARENTING TIPS PREGNANCY
PREGNANCY BABY CARE
BABY CARE TODDLERS
TODDLERS TEENS
TEENS HEALTH CARE
HEALTH CARE ACTIVITIES & CRAFTS
ACTIVITIES & CRAFTS