In a recent study published in the journal Seminars in Immunology, scientists review key studies on early-life microbial exposure and its impact on immunity and chronic inflammatory disease, particularly childhood atopy and asthma.
 Study: Contributions of the early-life microbiome to childhood atopy and asthma development. Image Credit: Lightspring / Shutterstock.com
Study: Contributions of the early-life microbiome to childhood atopy and asthma development. Image Credit: Lightspring / Shutterstock.com
The central role of the microbiome
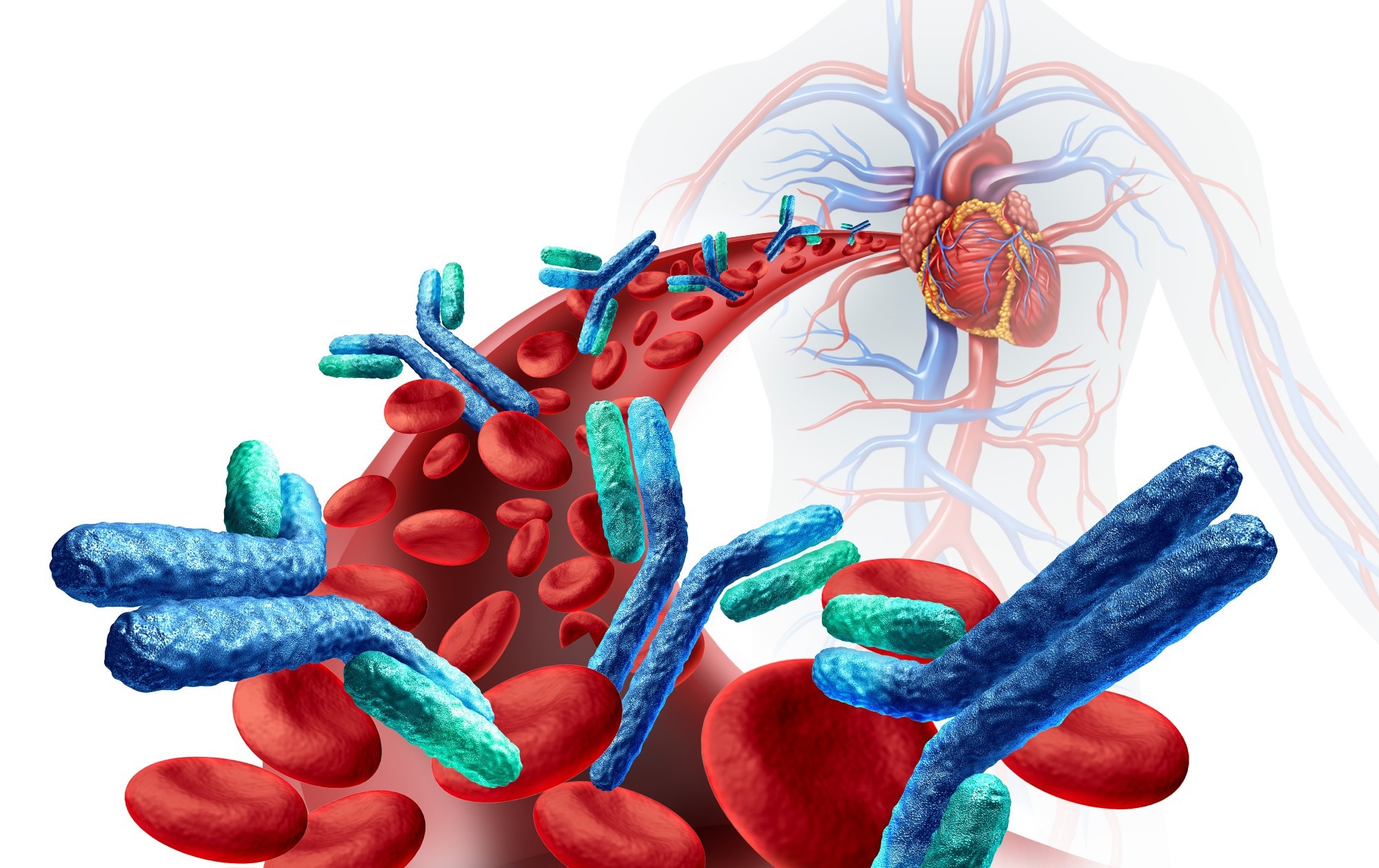
Most evidence in previous research indicates that all higher taxa depend on their microbiome for their persistence and propagation. This co-evolution of mutualism between higher biological entities and their microbiome has shaped ecosystem structure and function. A loss or alteration of the microbiome could potentially lead to ecosystem dysfunction, which, for humans, might manifest as immunosuppression or disease development.
The human holobiont, which is defined as the human host, in addition to the trillions of microbiota whose collective functioning keeps the whole assemblage alive, is characterized by a mutualistic relationship benefiting all participants. The human provides accommodation and nutrition to its microbiota, which offers their host an expanded genomic capacity, contributes to host immunity, and allows the holobiont to metabolize a broader range of nutritional and pharmacological substrates.
Research into the interactions between host and microbial cells is lacking; however, recent advancements in next-generation sequencing and mass spectrometry indicate a constant ‘molecular dialogue’ between microbial and mammalian cell populations.
These interactions appear to center around environmental factors such as host diet, pathogens exposure, and antimicrobials, as well as intrinsic factors including immunoglobulins, peptides, and mucins. Taken together, these factors alter microbiome composition and consequently disrupt normal gene function and immunity in unhealthy individuals as compared to healthy humans from the same population.
Research indicates that microbial disruptions can have long-term effects, as demonstrated by the ability of an altered gastrointestinal microbiota to impact the local organ system, as well as distant cardiovascular and neurological systems. Thus, host-microbiota dialogue might be leveraged to develop novel diagnostic and remedial tools. Nevertheless, such advancements must be preceded by a deeper understanding of the mechanisms underlying these mutualistic relationships.
Understanding the causes of childhood asthma and atopy
For several decades, researchers have been studying childhood atopy and asthma, as well as pre- and post-natal factors that appear to increase disease risk. In tandem with more recent scientific advances in molecular biology and mass spectrometry, these historic observations allow researchers to link activities that increase disease risk with specific microbiota assemblages, genes, or metabolic compounds.
Childhood asthma is complex, multifaceted, and generally respiratory tract-restricted; however, research has shown that both respiratory and gastrointestinal microbiome disruptions can contribute to the onset of the disease. This suggests that broader mucosal dysfunction from the earliest stages of life underlie disease development.
The impact of environmental and lifestyle factors
Despite the discovery and characterization of many genes that can trigger recurrent wheezing, recent increases in allergy prevalence in Western children indicate environmental and lifestyle changes contributing to disease development. Numerous studies have highlighted how, counterintuitively, reduced microbial exposure as an infant, especially in the ‘critical period’ from birth to two years of age, can significantly increase respiratory disease risk during childhood, potentially persisting life-long.
Industrialization, changing lifestyles, and medical choices in Western countries have been proposed as contributing factors to the rapid increase in allergy cases in these regions. Industrialization has altered environmental microbiota community composition, potentially reducing microbes that would naturally prime individuals’ immune systems during their early years.
Children raised on farms and less urban areas have significantly higher atopy and asthma resistance than their urban counterparts. Research on Amish and Hutterite populations, which share genetic ancestry, found that the former, who engage in traditional farming practices, exhibit a four-fold reduction in disease rates and significant differences in their white blood cell compositions when compared to Hutterites who engage in industrialized farming.
These observations have been attributed to the broader spectrum of microbiota exposure in non-urban areas, which were corroborated by studies performed on disease resistance in geographically adjacent, yet demographically distinct regions. For example, children living in Sonora, Mexico, and Russian Karelia were found to have four- and ten-fold higher resistance to allergies than those living in Arizona, United States, and Finnish Karelia, respectively. This difference has been attributed to the higher microbial load in the former groups’ drinking water as compared to their Westernized counterparts.
Lifestyle and medical choices, including those of vaginal versus cesarean births or type and number of pets, are relevant factors contributing to the risk of atopy.
Babies born vaginally, for example, have been shown to have their microbiomes derived primarily from that of their mothers and, as a result, are less likely to have asthma. Comparatively, cesarean-born infants are devoid of maternal microbiota and at a significantly increased risk of the disease. The number of household pets owned was found to be directly proportional to allergy resistance in children, with dogs imparting stronger resistance than cats.
Importantly, infants who experienced upper airway infections of Corynebacterium, Staphylococcus, or Alloiococcus were associated with a reduced risk of respiratory infections during childhood. In contrast, those that experienced Moraxella, Hemophilus, or Streptococcus infections were at a greater risk of childhood respiratory infections.
Conclusions
The study findings highlight the impacts of industrialization, as well as modern lifestyle and medical choices, on reduced disease resistance and increased likelihood of atopy and asthma in children, which may persist throughout their lives. These studies suggest maternal prenatal decisions and interventions before the years of life are essential in allergy prevention and boosting immunity.
Journal reference:
- Steininger, H., Moltzau-Anderson, J., Lynch, S. V. (2023). Contributions of the early-life microbiome to childhood atopy and asthma development. Seminars in Immunology 69. doi:10.1016/j.smim.2023.101795

 PARENTING TIPS
PARENTING TIPS PREGNANCY
PREGNANCY BABY CARE
BABY CARE TODDLERS
TODDLERS TEENS
TEENS HEALTH CARE
HEALTH CARE ACTIVITIES & CRAFTS
ACTIVITIES & CRAFTS