In a recent study published in the journal Nutrients, researchers review the impact of coronavirus disease 2019 (COVID-19) on the gut microbiota and microbiome-related immunity, as well as the use of nutritional interventions, including pre- and probiotics in reducing the susceptibility to COVID-19.
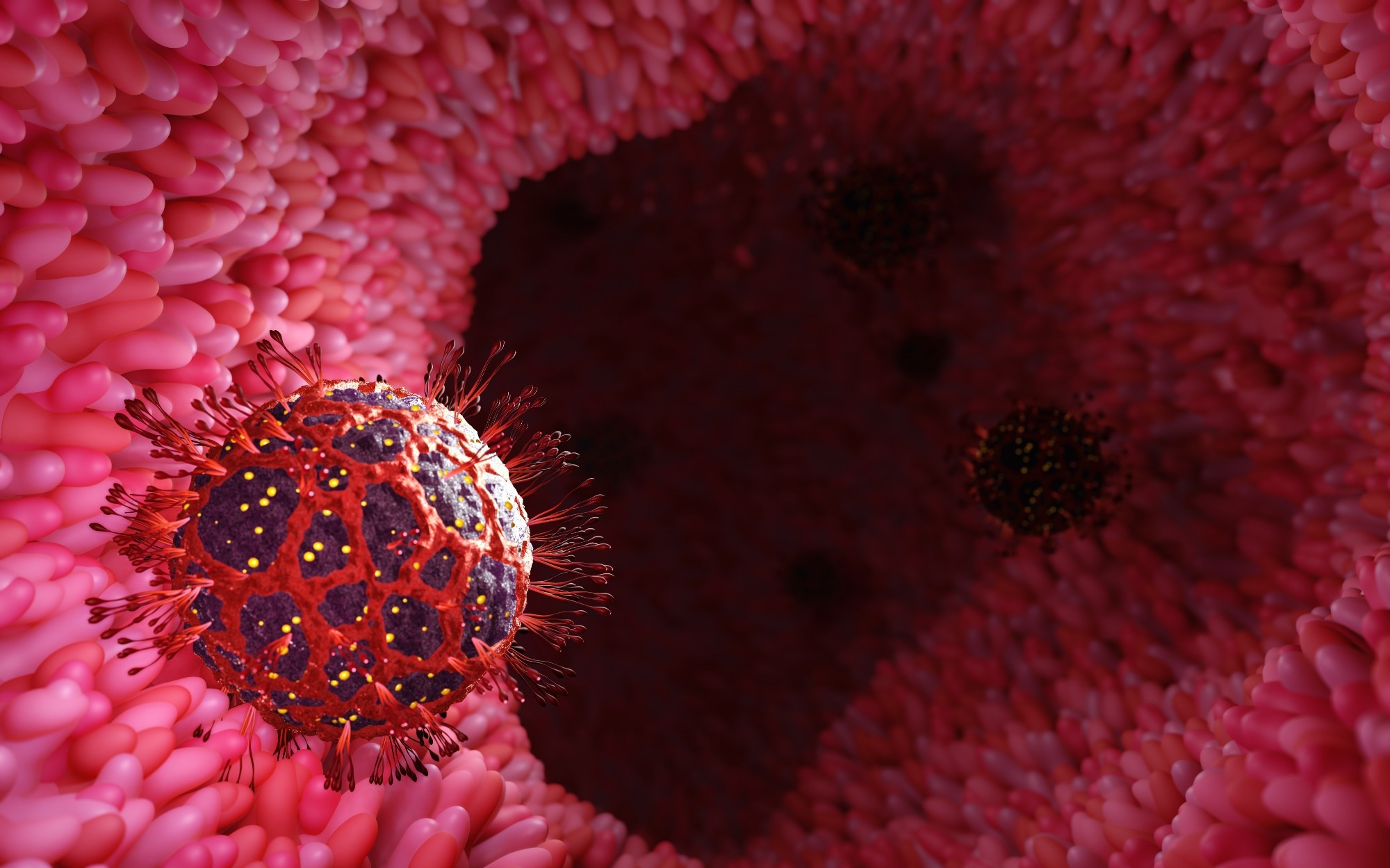 Study: Functional Foods: A Promising Strategy for Restoring Gut Microbiota Diversity Impacted by SARS-CoV-2 Variants. Image Credit: ridersuperone / Shutterstock.com
Study: Functional Foods: A Promising Strategy for Restoring Gut Microbiota Diversity Impacted by SARS-CoV-2 Variants. Image Credit: ridersuperone / Shutterstock.com
Background
Since the onset of the COVID-19 pandemic, growing evidence indicates that nutrition and supplementation with essential minerals and vitamins can significantly reduce the severity of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.
Vitamins C and D are known to improve the immune response against viruses and reduce cellular stress and levels of reactive oxygen species. Likewise, minerals such as zinc also contribute to the anti-viral response by enhancing the efficacy of anti-viral drugs and exerting their immune-protective effects.
In addition to severe respiratory symptoms, fatigue, fever, and dyspnea, between 2-21% of COVID-19 patients also experience gastrointestinal (GI) symptoms such as diarrhea, loss of appetite, nausea, and abdominal pain. Examinations of the gut microbiome of COVID-19 patients have revealed significant dysbiosis that increases their susceptibility to secondary infections in the respiratory and GI tracts.
The gut microbiome is crucial for processing and absorbing essential macro and micronutrients in the body, as well as supporting immune function. Thus, understanding the impact of COVID-19 on the gut microbiome and developing nutritional interventions to restore the microbiome balance can help reduce the severity of SARS-CoV-2 infection and subsequent secondary infections.
COVID-19 and the gut microbiome
The presence of SARS-CoV-2 ribonucleic acid (RNA) in stool samples indicates that the virus can infect the GI tract and spread through the fecal-oral route. Moreover, imaging techniques have revealed mesenteric thickening, hyperemia and bowel wall thickening, fluid-filled large intestine, and pneumatosis in patients with SARS-CoV-2 infections.
Diarrhea and nausea are the most common GI symptoms experienced by COVID-19 patients, with gut dysbiosis believed to be a major cause of these symptoms. Studies examining the gut microbiome of SARS-CoV-2 infected patients revealed a decrease in the abundance and diversity of beneficial bacteria such as Faecalibacterium, Roseburia, and Eubacterium and subsequent increase in species such as Clostridium hathewayi, Coprobacillus, and Clostridium ramosum that show positive associations with disease severity.
Dysbiosis, which involves the loss of beneficial gut microbes, loss of overall microbial diversity, and increased abundance of pathogenic bacteria, is associated with various other chronic diseases. Changes in the gut microbiome increase the risk of other comorbidities such as Alzheimer’s disease, hypertension, asthma, and dementia, as well as an altered immune system, the latter of which can increase an individual’s risk of severe SARS-CoV-2 infection.
The age-related decrease in gut microbial diversity has also been implicated in the increased severity of SARS-CoV-2 infection in elderly patients. Obesity, which also has significant associations with gut microbiome dysbiosis, is also correlated with severe COVID-19 outcomes.
Other risk factors such as diabetes and hyperglycemia, and cancers are also known to cause gut microbiome dysbiosis, which contributes to the increased susceptibility of diabetes and cancer patients to COVID-19.
Therapies and interventions
Antiemetic and antidiarrheal medications can be used to address nausea and diarrhea associated with COVID-19, along with regular rehydration and monitoring of potassium levels. Additionally, increasing beneficial gut bacteria through the consumption of plant proteins, polyphenols, complex polysaccharides, and micronutrients may improve COVID-19 outcomes by increasing the production of short-chain fatty acids (SCFAs) needed for immune system regulation.
GI symptoms of COVID-19 can also be alleviated by prebiotic intake, which helps restore the gut microbiome balance. The use of prebiotics, which consist of fibers that increase gut fermentation and beneficial gut bacterial growth, has been popular in various traditional medicine forms and addressing GI problems such as diarrhea and constipation.
Probiotics help break down the various fibers that constitute prebiotics, which subsequently leads to the production of SCFAs that activate G-protein coupled receptors and influence the activities of various immune cells, such as macrophages, T-cells, and dendritic cells. Certain probiotic bacteria also exhibit anti-viral properties against other coronaviruses.
Various natural compounds and herbal formulations are also being explored for their efficacy in reducing the severity of SARS-CoV-2 infection. These formulations often contain bioactive compounds such as alkylamides, curcuminoids, and alkaloids that have anti-inflammatory and anti-viral properties.
Conclusions
The current study provides a comprehensive understanding of the impact of COVID-19 on the gut microbiome and the subsequent increase in susceptibility to severe SARS-CoV-2 infection due to the detrimental effects of gut microbiome dysbiosis on immune function.
The researchers also discussed the various therapeutic interventions such as probiotics, prebiotics, herbal formulations, and functional foods that can be used to restore the balance of the gut microbiome, thereby improving immune system function and resilience against severe COVID-19 outcomes.
Journal reference:
- Banerjee, A., Somasundaram, I., Das, D., et al. (2023). Functional Foods: A Promising Strategy for Restoring Gut Microbiota Diversity Impacted by SARS-CoV-2 Variants. Nutrients 15(11). doi:10.3390/nu15112631

 PARENTING TIPS
PARENTING TIPS PREGNANCY
PREGNANCY BABY CARE
BABY CARE TODDLERS
TODDLERS TEENS
TEENS HEALTH CARE
HEALTH CARE ACTIVITIES & CRAFTS
ACTIVITIES & CRAFTS

