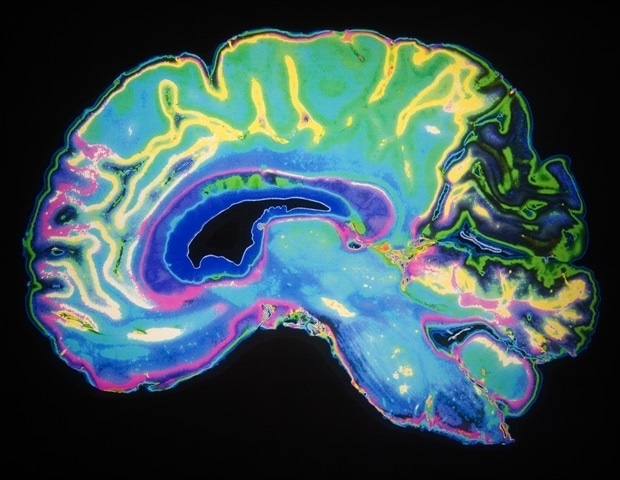
Obesity is a growing epidemic in children and adults. A large national study published in the International Journal of Obesity now finds that preteens carrying excess weight have notable differences in cognitive performance, brain structures, and brain circuitry when compared to preteens with normal body-mass index (BMI).
Funded by the National Science Foundation’s Harnessing the Data Revolution initiative, the study involved nearly 5,000 9- to 10-year-olds at 21 sites across the United States. While it only examines the relationship between BMI and the brain and cannot establish causation, there is a significant association between BMI and brain measures in the study.
Study leader Caterina Stamoulis, PhD, a researcher in Adolescent Medicine and director of the Computational Neuroscience Laboratory at Boston Children’s Hospital, finds the association concerning.
It raises an alarm that it’s important to track adolescents’ brain health, especially when they have excess BMI. Early adolescence is a time when the brain is very actively developing, and when frontal areas of the brain -; those involved in higher cognitive functions -; change enormously and are vulnerable to miswiring.”
Caterina Stamoulis, PhD, Study Leader
Inefficiently organized brain networks
The study drew its subjects from the government-funded Adolescent Brain Cognitive Development (ABCD) study, which has collected detailed clinical, physiological, environmental, and lifestyle information, together with neuroimaging and neurocognitive data. Stamoulis and colleagues in her lab use advanced computational methods to analyze the large data sets.
In preteens with excess BMI, brain circuits supporting higher-level cognitive functions, reward, emotional processing, and attention were found to be organized less efficiently, less well connected, and less resilient than in preteens with normal BMI.
Excess BMI was correlated with difference in multiple brain structures, as well as a lower ability to think logically and solve problems in new settings. The differences were consistent even after adjusting for factors like sleep duration, screen time, physical activity, depression, and self-worth related to weight that may affect both BMI and brain health.
Whether BMI plays a direct causative role or not in brain development, Stamoulis emphasizes that preteens’ brains are still changing, and that interventions can make a difference -; whether they be mental health screenings, improving sleep quantity and quality, increasing physical activity, or reducing screen time.
A stake in the ground
Stamoulis now plans to analyze two-year follow-up data from additional waves of the ABCD datasets to see what happens to the brains of kids with excess BMI over time. “Once the brain is done wiring, it’s more difficult to intervene,” she says. “We want to see what neurodevelopmental trajectories these youth are on.”
She also hopes to analyze genetic and nutritional data, which the ABCD study plans to release in the future.
Source:
Boston Children’s Hospital
Journal reference:
Brooks, S. J., et al. (2023). Excess BMI in early adolescence adversely impacts maturating functional circuits supporting high-level cognition and their structural correlates. International Journal of Obesity. doi.org/10.1038/s41366-023-01303-7.

 PARENTING TIPS
PARENTING TIPS PREGNANCY
PREGNANCY BABY CARE
BABY CARE TODDLERS
TODDLERS TEENS
TEENS HEALTH CARE
HEALTH CARE ACTIVITIES & CRAFTS
ACTIVITIES & CRAFTS