Childhood asthma is a condition that may be affected by different types of factors. These include the state of the infant’s gut microbiome, environmental factors, and genetic factors. A recent study attempted to shed more light on how asthma risk is linked to a combination of these factors, some of which are modifiable.
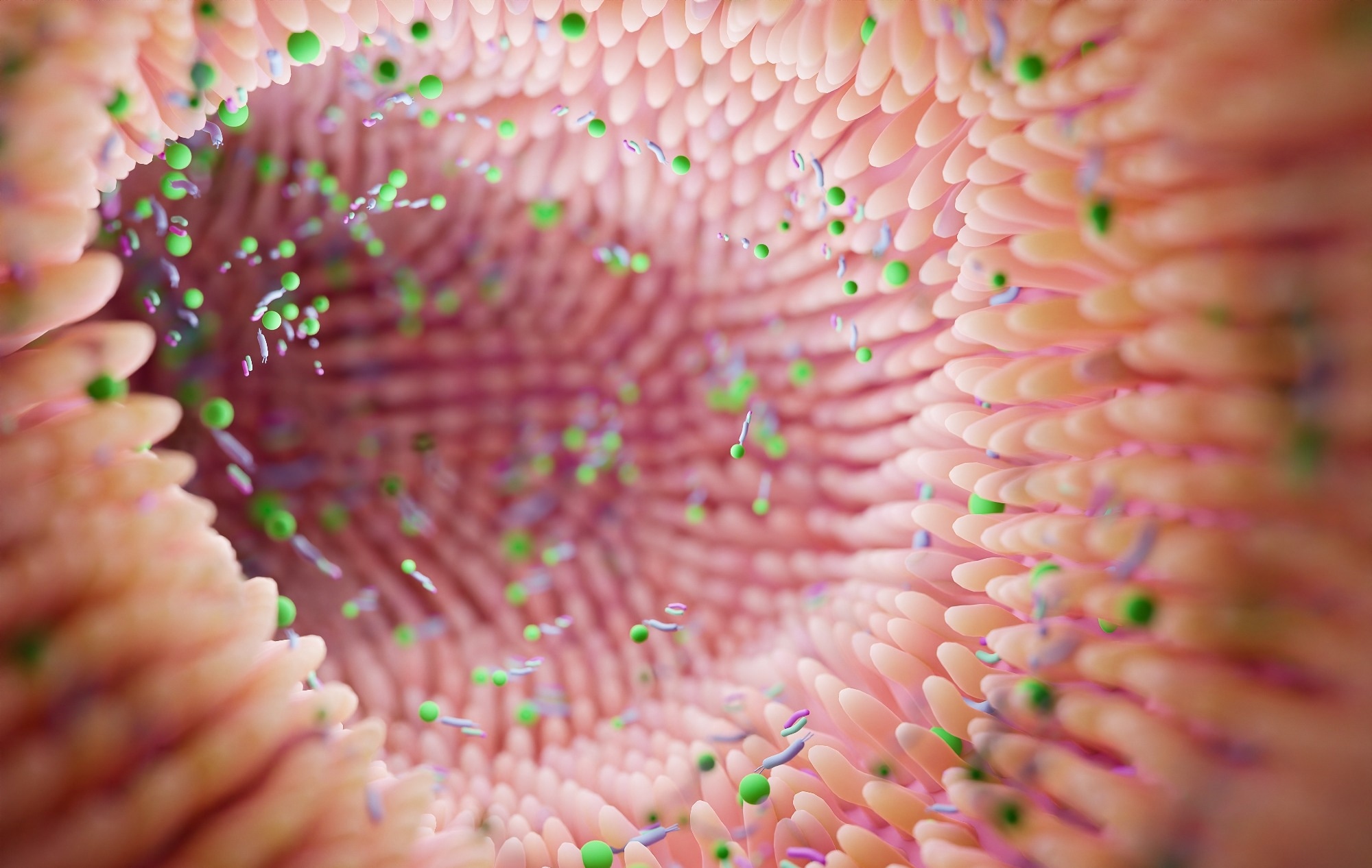 Study: Environmental and genetic associations with aberrant early-life gut microbial maturation in childhood asthma. Image Credit: Troyan / Shutterstock
Study: Environmental and genetic associations with aberrant early-life gut microbial maturation in childhood asthma. Image Credit: Troyan / Shutterstock
Introduction
The gut microbiome is now known to mediate or contribute to a significant proportion of cases of atopy. This includes the composition and maturation of the microbiome at birth and during infancy. The risk of atopy has also been linked to the 7q12-21 gene locus, associated with factors that drive the gut microbiome composition, such as growing up on a farm or having older siblings.
It is necessary to identify the factors that determine how the gut microbiome matures in infancy to potentially prevent the future development of atopy.
In the current study, published in the Journal of Allergy and Clinical Immunology, the scientists examined samples of the gut microbiome from >460 infants aged 3-6 months and one year of age. These were the children of parents who had participated in the Vitamin D Antenatal Reduction Trial (VDAART). They looked for potential links between the gut microbiome and genetic factors in these infants and the risk of asthma at the age of three years.
The researchers used longitudinal fecal 16s rRNA (ribosomal ribonucleic acid) samples from these children, taken at 3-6 months, one year, or both. They also examined the presence of wildtype or mutational 17q12-21 genotypes in association with asthma risk and microbial maturation in the above cohort and the Copenhagen Prospective Studies on Childhood Asthma 2010 (COPSAC). These cohorts differ in that the biological mother in the former cohort had atopy or asthma.
The child had to be diagnosed with asthma or recurrent wheezing by this time point by a physician to be eligible for this study. The study also explored contributions by the differences in the genera Bifidobacterium and Bacteroides, which have been reported to be linked with the mode of delivery and breastfeeding.
What does the study show?
Children more likely to have asthma were less likely to be from the San Diego arm of the study, to have pet dogs, or to be breastfed, and more likely to be Black and to have been given antibiotics around the time of childbirth compared to those without asthma (53% vs. 39%, respectively).
The findings of this study show that children at a higher risk of childhood asthma at three years were more likely to show rapid maturation of the fecal microbiome at 3-6 months or a lag in the maturation of this microbiome at one year.
Increased and decreased Bifidobacterium abundance at 3-6 months was linked to breastfeeding and higher microbial maturity. This supports the observation of this study that breastfed infants show delayed microbial maturation at this time point.
Similarly, Bacteroides abundance at 3-6 months was associated with breastfeeding and lower abundance with Cesarean section at both time points. Bacteroides abundance was thus linked to faster maturation of the gut microbiome at one year of age.
Children with asthma at three years were 70% less likely to have had Bacteroides in their fecal samples at 3-6 months and >30% less likely at one year. They were also more likely to have low Bacteroides abundance at 3-6 months than those without asthma.
Slow maturation at 3- 6 months was more likely among breastfed infants. Over 60% of the association of asthma risk with breastfeeding was found to be due to the association of the latter with better microbial maturation at 3-6 months.
Babies born by Cesarean section rather than vaginally were more likely to show delayed maturation of the microbiome at one year, though not at the earlier time point. These results seem to buttress the favorable role of breastfeeding and vaginal delivery in reducing the risk of asthma.
Antibiotic exposure and having owned pets were not significantly linked to microbial maturation. Environmental effects mediated by the maturation of the fecal microbiome were found to act independently of but in addition to genetic factors.
The 17q12-21 risk alleles rs12936231 and rs8076131 carried a 30% and 25% increased risk of asthma when adjusted for race and ethnicity.
When both alleles were present with increasing microbial maturation at 3-6 months, the risk of childhood asthma was increased by over threefold. At this age, half the subjects with at least one risk allele at rs12936231 and accelerated maturation developed asthma, but only 6% with neither of these factors, showed an increase in risk by almost 20 times. The risk was increased by 6.5-fold if an rs8076131 risk allele was present along with aberrant maturation vs. no risk factors.
If only microbiome or genetic factors were present, the risk was six-fold and 3.5-fold, respectively, compared to no risk factor. These patterns were repeated for one year. The order of increase in risk goes from no genetic or microbiome risk<genotype risk<microbiome risk<both factors (double risk).
What are the implications?
This study’s findings show that aberrant gut microbiome maturation in infants is responsible for the known association of asthma with environmental factors like breastfeeding. In addition, the VDAAR cohort included mothers with atopy or asthma, which causes the fetal immune system to be imprinted without actual genetic alteration.
“Infants who develop asthma are more likely to deviate from normal microbiome development over the first year of life, and these differences in microbial maturation may be affected by modifiable exposures such as breastfeeding.”
Environmental exposures seem to affect the maturation of the infant microbiome, modulating asthma risk. Factors affecting microbial maturation included breastfeeding and mode of delivery, and the maturation itself was indicated by differential abundances of two key species, Bacteroides and Bifidobacteria.
However, genetic factors, especially the nature of the genes at the 17q12-21 locus, show an additive effect that acts independently of the environmental factors. This contradicts some earlier studies, underlining the complex interrelationships of these risk factors. More extensive studies with more extended and more frequent examinations of the microbiome will help explain these relationships better.

 PARENTING TIPS
PARENTING TIPS PREGNANCY
PREGNANCY BABY CARE
BABY CARE TODDLERS
TODDLERS TEENS
TEENS HEALTH CARE
HEALTH CARE ACTIVITIES & CRAFTS
ACTIVITIES & CRAFTS

