[ad_1]
Although severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), the causal agent of coronavirus disease 2019 (COVID-19) pandemic, does not affect children widely, rare events of the multisystem inflammatory syndrome in children (MIS-C) have been reported. Scientists have stated that MIS-C is a severe, post-infection hyperinflammatory condition that typically occurs two-six weeks after COVID-19 infection. During pre-Delta SARS-CoV-2 waves, MIS-C was reported in 1 in 3,000–4,000 children infected with the SARS-CoV-2 virus. All these children were unvaccinated.
Scientists have worked extensively hard to protect all individuals from COVID-19 infection. Although several COVID-19 vaccines initially received emergency use authorization (EUA) for vaccinating adults, the BNT162b2 vaccine, developed by Pfizer–BioNTech, received approval from the European Medicines Agency for vaccinating children.
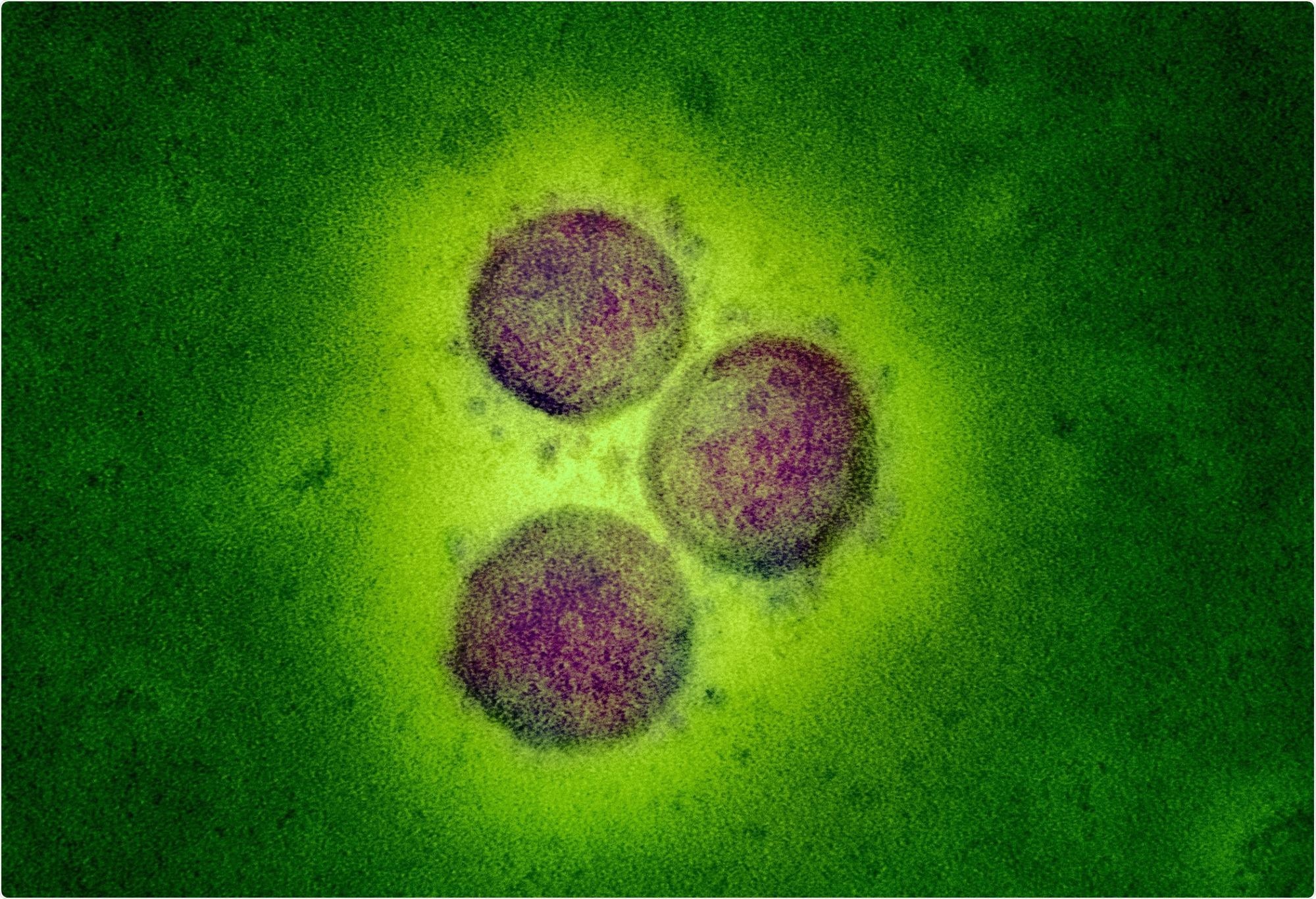 Study: Incidence and clinical phenotype of multisystem inflammatory syndrome in children after infection with the SARS-CoV-2 delta variant by vaccination status: a Danish nationwide prospective cohort study. Image Credit: NIAID
Study: Incidence and clinical phenotype of multisystem inflammatory syndrome in children after infection with the SARS-CoV-2 delta variant by vaccination status: a Danish nationwide prospective cohort study. Image Credit: NIAID
Background
Previous studies have determined several factors associated with the incidence of MIS-C, which include the effectiveness of COVID-19 vaccines, the virulence of SARS-CoV-2 variants, and the effectiveness of the available vaccines against MIS-C after breakthrough infection. During the SARS-CoV-2 Delta wave, studies conducted in France and the USA reported a high vaccine efficacy against MIS-C in young adults. However, the underlying mechanisms behind these results are not clear. For instance, these studies failed to elucidate if adolescents exhibited a reduced risk of MIS-C owing to vaccination or breakthrough infections, or both. Also, not much evidence is available to prove that all SARS-CoV-2 variants pose the same risk of MIS-C similar to pre-Delta variants.
Denmark experienced a rapid increase in COVID-19 cases after the emergence and circulation of the Delta variant, i.e., from July to December 2021. It developed a nationwide SARS-CoV-2 surveillance system that contained COVID-19 test results from both public and private providers. The surveillance system also included details of vaccination status for each individual via a unique registration number.
A New Study
Researchers designed a nationwide pediatric COVID-19 research project based on real-time data since the early phase of the pandemic. They collected data on phenotypes of COVID-19-associated diseases, including MIS-C manifestations. The main focus of this research was to assess the incidence of MIS-C and to define its clinical phenotype after the participants were infected with the Delta variant. In addition, researchers also considered their vaccination status. Interestingly, the authors also compared the rate of incidence of MIS-C during the period when the Delta variant circulated from the pre-Delta era. This study is available in the journal Lancet Child and Adolescent Health.
In this study, researchers included COVID-19 patients whose ages were between zero and seventeen. All the patients were hospitalized between August 1, 2021, and February 1, 2022, when the Delta strain was dominantly circulating in Denmark.
Key Findings
The current study revealed the incidence of MIS-C after SARS-CoV-2 Delta infection to be 1 in 3,400 infected unvaccinated children and young adults. This result is comparable to the estimated MIS-C infection during the pre-Delta period, i.e., one in 3,000–4,000 unvaccinated children.
Importantly, researchers reported that two doses of Pfizer–BioNTech vaccines exhibited 94% efficacy against MIS-C. This estimate was found to be similar to the US data, where the Pfizer–BioNTech vaccine exhibited 91% effectiveness against MIS-C.
Scientists provided two explanations regarding reduced MIS-C incidence in vaccinated children and adolescents. They stated that COVID-19 vaccines might have offered substantial protection against SARS-CoV-2 infection, putting fewer children and adolescents at risk of developing MISC. Another explanation was that vaccines could have a direct effect on the susceptibility of MIS-C after breakthrough infection, which might be because of the fact that vaccine-induced immune protection could prevent hyperinflammation.
Even though the current study found that the incidence of MIS-C due to the Delta variant was similar to the original SARS-CoV-2 variant, the Omicron variant is phylogenetically distant and might cause differential MIS-C incidence. Researchers also highlighted the risk of MIS-C after reinfections. For instance, many children were found to have contracted SARS-CoV-2 infection twice, and hence, reinfection could affect the magnitude of MIS-C manifestation.
Interestingly, male children were found to be more susceptible to MIS-C compared to females. In the study cohort, 73% of male children and young adults suffered MIS-C after being infected with the Delta variant and 61% after being infected with the original SARS-CoV-2 strain.
Conclusion
The study’s main limitation is the low number of cases of MIS-C in the study cohort. However, the key strength is its nationwide pediatric research set-up containing real-time data consisting of detailed phenotyping and vaccination status of the study cohort. The authors stated that it is vital to understand the impacts of COVID-19 vaccination so that parents can make an informed decision regarding vaccinating their children.
[ad_2]
Original Source Link

 PARENTING TIPS
PARENTING TIPS PREGNANCY
PREGNANCY BABY CARE
BABY CARE TODDLERS
TODDLERS TEENS
TEENS HEALTH CARE
HEALTH CARE ACTIVITIES & CRAFTS
ACTIVITIES & CRAFTS

