During pregnancy, the mother experiences a wide range of physiological changes to ensure that the fetus grows and develops normally while keeping her body healthy.
One such change is adapting to the increased stress associated with pregnancy by neutralizing potential damage due to the release of oxidative molecules. This involves biological rhythms set to the day-night cycle to optimize the chances of survival.

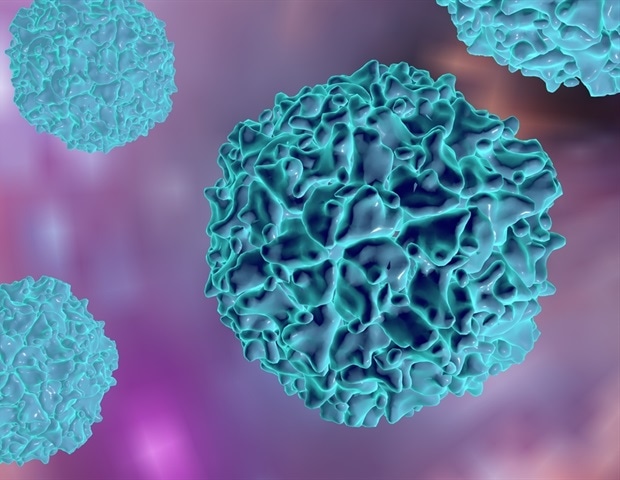
Study: The role of Melatonin in Pregnancies Complicated by Placental Insufficiency: A Systematic Review. Image Credit: Pressmaster / Shutterstock.com
A new European Journal of Obstetrics and Gynecology and Reproductive Biology study explores the role of melatonin. This molecule is key to several vital physiological processes that also possesses anti-inflammatory and antioxidant properties in pregnancy.
What is melatonin?
Circadian rhythms typically correspond to and follow the normal light-dark cycle throughout the day. These rhythms are important in regulating biological functions to ensure that they occur at the right time of day relative to the environment.
The disruption of circadian rhythms has been associated with adverse pregnancy outcomes that are more frequent in women suffering from jetlag or those who work night shifts. Altered circadian rhythms during pregnancy also contribute to the development of cardiovascular illnesses by promoting hypertension, which can also reduce blood flow to the uterus and developing fetus.
The hypothalamus’s suprachiasmatic nuclei (SCN) mediate the circadian rhythm through neurotransmitters that act on specific proteins in peripheral tissues. Melatonin, for example, regulates the sleep-wake cycle and promotes cell survival by averting oxidative damage, thus preventing apoptosis and reducing inflammation.
Melatonin production during pregnancy
Melatonin was previously thought to arise from the pineal gland, located deep in the brain; however, recent studies suggest its production is localized to the placental villi. During pregnancy, melatonin is secreted rhythmically, with higher levels produced at night.
There is a slight decrease in melatonin production in the first two trimesters of pregnancy, followed by its peak production at 32 weeks. After childbirth, melatonin levels rapidly decline.
Melatonin scavenges free radicals directly and through its many metabolites. This hormone also increases the activity of glutathione peroxidase and other antioxidant enzymes.
The importance of melatonin activity at the placental level is demonstrated by the expression of melatonin receptors MT1 and MT2 in this tissue. Melatonin is fat-soluble and crosses the cell membrane to scavenge free radicals independent of these receptors in an autocrine manner to produce rapid antioxidant effects. This might explain why placental melatonin production is independent of the circadian rhythm, unlike pineal melatonin secretion, thus protecting the placenta from oxidative stress.
Melatonin levels in pregnancy peak at 32 weeks, perhaps to protect the aging placenta from increased oxidative stress due to the needs of the rapidly growing fetus. In vitro studies have also indicated that the antioxidant activity of melatonin could promote placental health by preventing apoptosis.
In pregnancies with placental insufficiency, impaired remodeling of the spiral arteries during the initial establishment of the placenta leads to inadequate placental angiogenesis and placental ischemia followed by reperfusion. The subsequent damage increases the release of reactive oxygen species (ROS).
Reduced melatonin levels disrupt antioxidant protective signaling pathways, thus promoting placental damage. The impaired trophoblastic function is not rescued by melatonin, thus predisposing the mother to pre-eclampsia and fetal growth restriction (FGR).
Melatonin supplementation in animals has been shown to reduce blood pressure, promote angiogenesis, increase uterine artery blood flow, and enhance serum antioxidant capacity. These reports have increased interest in using melatonin to potentially prevent and treat pregnancy disorders related to placental insufficiency, including pre-eclampsia and FGR. Both have been linked to more significant oxidative damage and inflammatory stress.
The current study reviews available literature on the role of melatonin in pregnancy complicated by placental insufficiency relative to its preventive effect on these disorders. The researchers reviewed 12 original studies on melatonin in pre-eclampsia, FGR, and other related conditions.
This is the first systematic review to examine how melatonin affects pregnancies complicated by placental insufficiency.
Study findings
Four studies showed lower circulating melatonin levels in maternal blood in pregnancies complicated by pre-eclampsia, with low levels being proportional to severe pre-eclampsia in late pregnancy. However, one study reported increased melatonin levels in pre-eclampsia pregnancies compared to controls.
Melatonin levels were also found to be lower in pregnancies with FGR; however, this was only reported in one study. Another study of twin pregnancies that later developed FGR showed no difference in serum melatonin levels in the first trimester.
Melatonin M1 and M2 receptors in the placenta were reduced in pre-eclampsia pregnancies, while the precursor molecule serotonin was elevated. This was likely due to the downregulation of placental genes for melatonin expression, along with the suppression of genes encoding the enzymes for serotonin conversion to melatonin in the chorionic villi. Both receptors were also reduced in FGR pregnancies.
The limited available data indicates the safety of melatonin administration for both the mother and fetus. In addition, administration of 30 mg/day prolonged the delay to delivery from the point of pre-eclampsia diagnosis by almost one week, which is essential for fetal maturation.
Meanwhile, pre-eclampsia-related hypertension was controlled with fewer drugs. However, this finding depended on historical controls rather than a randomized controlled trial.
The same benefit of melatonin supplementation was not observed with FGR pregnancies. More specifically, no significant improvement in birth weight following melatonin supplementation was reported. However, placental oxidative markers were reduced, as indicated by lower lipid peroxidation metabolite malondialdehyde (MDA) levels.
Implications
In pregnancies complicated by placental insufficiency, serum melatonin levels in pregnant women are lower. In addition, placental melatonin receptors are also significantly reduced in these cases.
The underlying phenomenon appears to be an altered pattern of melatonin secretion that is mediated by changes in the physiological and circadian rhythms. The resulting decrease in melatonin secretion reduces circulating melatonin levels in both systemic and placental circulation. Furthermore, the accompanying downregulation of melatonin receptors in the placenta reduces the local release of melatonin, thereby impairing its autocrine protective function.
Some preliminary studies indicate that melatonin administration could improve placental levels of this molecule in pregnant women and increase glutathione peroxidase concentrations. However, there is limited clinical evidence that this could reduce the incidence of pre-eclampsia and FGR.
Further research is needed to understand the potential role of oral melatonin supplementation in preventing adverse pregnancy outcomes or improving such outcomes. Two ongoing randomized controlled trials are currently examining the benefit of melatonin in preventing pre-eclampsia in high-risk women and improving neurodevelopmental outcomes in infants with FGR.
Journal reference:
- Fantasia, I., Bussolaro, S., Stampalija, T., & Rolnik, D. L. (2022). The role of Melatonin in Pregnancies Complicated by Placental Insufficiency: A Systematic Review. European Journal of Obstetrics and Gynecology and Reproductive Biology. doi:10.1016/j.ejogrb.2022.08.029.

 PARENTING TIPS
PARENTING TIPS







 PREGNANCY
PREGNANCY








 BABY CARE
BABY CARE






 TODDLERS
TODDLERS








 TEENS
TEENS








 HEALTH CARE
HEALTH CARE




 ACTIVITIES & CRAFTS
ACTIVITIES & CRAFTS








 CONTACT
CONTACT ABOUT
ABOUT













